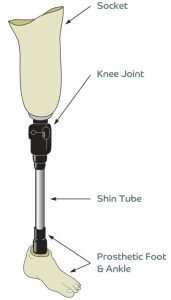
What are the parts of a prosthesis?
Above knee: also called transfemoral
Below Knee: also called transtibial

Use of prosthesis:
You will need to get used to wearing your prosthesis and allow your skin to adjust.
Initially we ask that it is worn for 30 mins twice a day (e.g. am and pm) for a week. If your skin tolerates this and does not cause pain or red marks, then this can be increased to1 hour twice a day after a week. This continues to gradually build up week on week as long as no issues arise until eventually you put the prosthesis on in the morning and keep it on until the evening.
Initially you may be asked not to walk with your prosthesis at home, but to sit with it on or do standing activities without stepping. Your therapy team and Prosthetist will let you know what you should be doing after each treatment session and this will increase gradually.
When you put on your limb you have to assess each time how many socks you need – this will vary day to day as your residual limb size my increase and decrease. If your residual limb increases and you cannot put your prosthestic limb on without pinching/good fit then you should remove it, and put your Compression sock on, elevate the limb and rest it out straight to help reduce the size. If it still does not go down then you should not wear it that day.
If the residual limb size goes down then please refer to the sock leaflet on how to manage.
There may be days when the limb does not fit at all and can be due to a variety of reasons including and not limited to; the weather, being unwell, changes in weight and other health issues.
Suspension
To keep your prosthesis on you and in place while walking there are several methods of suspension to facilitate this.
Initially for above knees it may be an elasticised strap that does up around your waist, and for below knee a silicon sleeve or a buckle fasten strap that goes up over your knee.
If the strap is not done up tightly enough it can make the prosthesis feel unsecure on you while walking.
For sleeves they should be in contact with your skin and go up above the height of your white socks. If this does not happen the sleeve will not suspend.
When putting a suspension sleeve on we recommend that you roll the sleeve up rather than pull it up as this can lead to tears in the silicon and allow air to escape and suspension to be reduced or fail.
Always take the time to ensure these are on correctly before you walk.
Care of prosthesis:
In order to look after your prosthesis you should aim to clean the pelite liner, gel/silicon liners, suspension sleeves daily to reduce risk of bacterial build up. To do this, use a damp cloth with soapy water and wipe down the surfaces that contact your skin. Allow to fully dry before wearing again. This is ideal at the end of the day, or may need to be done more regularly if your stump becomes sweaty.
Alternatively baby wipes can be used to clean the inside.
Socks should also be washed daily on 30 or 40 degree wash and dried naturally not in a tumble dryer.
You should attend your routine appointments with your prosthetist to check the fit and that the mechanics stay optimal. If you are having issues with fit, something breaks, or is not right, please contact the department sooner, your appointment can be brought forward if needed, or the issue can be discussed on the phone with the team.
Footwear and alignment
Your prosthesis is set up at a certain height to optimise your ease of walking.
Therefore you should aim to keep the heel height (sole height) of your shoes similar. If your change shoes on your prosthesis and you wear something much flatter or more elevated than what was worn in set up, it may affect your walking and make you feel pressure in your residual limb or put more strain on your back.
If you need to wear a different heel height, please speak with your prosthetist as they can adjust your prosthesis.
You should avoid wearing your prosthesis with bare feet indoors, you should use your shoes or change into a pair of full backed slippers i.e. not backless mule style
Skin issues for bad fit
If you do not adjust your socks properly or ignore sore points, this can lead to skin problems that may mean you are unable to wear the prosthesis at all. Poor fit can lead to blisters, grazes, pressure areas and infected wounds. If you feel fit is not correct and cannot be changed by adjusting your socks, suspension or donning process then please do not ignore the symptoms, contact the centre for advice.
Residual limb care
Ideally you should shower or wash in the evening so that your skin is fully dry when you put your prosthesis on.
Keep your residual limb moisturised and your scar smooth and free moving with massage techniques taught to you by the Physiotherapist.
We recommend that you do not use hair removal creams or shave the hair on your residual limb as this opens the pores up and then they are enclosed in a hot, dark and potentially damp environment. If cosmetically this is an issue you can consider laser hair removal.
You should check your residual limb for any grazes, cut, blisters etc regularly, you may need a handheld mirror to see the underside of your residual limb clearly.
Sweating is a possible side effect to prosthesis use. If this affects you, then speak with the prosthetist or rehab team and they can recommend creams aimed to reduce sweat, or consider alternative liners etc if creams fail.
You may need to remove your prosthesis for a period in the day to dry your stump/liner/socket and may need to swap to fresh socks.
Energy consumption for walking
Using a prosthesis is more draining than how your walked pre amputation. Due to the lost of muscles from the amputation your remaining muscles have to do more and work harder to compensate for those lost.
Roughly below knee amputee’s remaining muscles work 20-50% more and above knee amputee’s work approximately 70-90% more.
As a result you may fatigue quicker than pre amputation, may not be able to walk as far as previous, and may need new or additional walking aids to help you e.g. if you used a walking stick pre amputation you may need two post amputation or a frame. Your therapy team will monitor your progress and assess your walking regularly and provide assistance/aids/equipment as needed.
Secondary Issues
If your prosthesis does not fit correctly, or you walk in an unadvised manner or with the incorrect walking aids, it can lead to secondary problems like low back pain, hip or knee pain. As your muscles will be working in an inefficient manner and compensating and overworking in different areas, which can lead to musclo-skeletal problems like bursitis, sciatica, flare ups in Osteoarthritis and muscles strains.
