What is an ERCP?
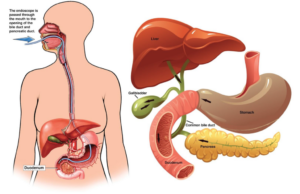
The examination you will be having is called an ERCP which stands for Endoscopic Retrograde Cholangio-Pancreatography. This procedure enables the doctor to examine the common bile duct and the pancreatic duct. The instrument used is a long, flexible tube about the same thickness as your finger with a light on the end called a duodenoscope. It also has a very small camera which sends a live image to a screen, where it is viewed by the doctor. The examination is carried out by a specially trained doctor called an endoscopist. During the ERCP, the endoscopist will also use X-rays and a special dye to show up your bile ducts on the screen.
In order to carry out this procedure the duodenoscope will be passed through your mouth down into the stomach and the first part of your small bowel (the duodenum) at the point where the bile duct and pancreatic duct drain into the small bowel.
ERCP is used mostly to diagnose and treat conditions of the bile ducts and pancreas.
Why do I need an ERCP? What are the benefits?
Your doctor is concerned that you may have problem or a blockage in your bile duct or pancreatic duct. Gallstones or narrowing in your bile duct are common problems, both which can cause jaundice (your eyes and skin turning yellow)
An ERCP may be recommended for a number of reasons, including to:
- Help your doctors to make a diagnosis.
- Treat jaundice caused by gallstones or narrowing of bile ducts
- Remove stones from the bile ducts or pancreatic ducts
- Insert a plastic or metal tube to drain the bile (or the pancreatic juices)
- Clear blockage of the bile flow
What are the risks and complications?
- Acute Pancreatitis: Injection of dye into the pancreatic duct can occasionally cause inflammation of the pancreas known as pancreatitis. The risk of this occurring is approximately 5%
- Bleeding: This can occur in 1 in 500 patients but is 10 times more likely (10 in 500) if a cut has been made (sphincterotomy) to remove stones or to insert a stent.
If the x-rays show a gallstone the doctor will enlarge the opening of the bile duct (Sphincterotomy). This is done with an electrically heated wire (diathermy) which you will not feel. This procedure carries a 1% risk of significant bleeding but this risk is minimised by checking your blood clotting results before the procedure. If bleeding occurs, you may need a blood transfusion and very occasionally an operation to stop the bleeding.
If a sphincterotomy is performed, pancreatitis may also occur, again with a risk of approximately 5%. If a narrowing is found, bile can be drained by leaving a short plastic tube (stent) in the bile duct.
Occasionally it may be necessary to replace or remove the tube some months later if it becomes blocked.
- Perforation: A tear in the gastrointestinal wall or bile system occurs very rarely (1 in 1000 patients), which might require surgery to be repaired.
- Small abnormalities may be missed, although this is unlikely.
- Adverse reaction to the sedation medication or the X-ray dye.
- Short term problems with breathing, heart rate and blood pressure (related to sedation). You will be monitored closely so that if any problems do occur, they can be treated quickly.
- Heart attack or stroke (related to sedation)- though this is very unlikely
- Damage caused by the duodenoscope to teeth or bridgework– this is very rare
Please remember that these procedures and the risks are much safer than the only other option which is to have a full operation.
Are there any alternatives to an ERCP?
There are other ways of looking at your bile duct such as a Computed tomography (CT) and magnetic resonance imaging (MRI), or a technique called endoscopic ultrasound. These investigations can also provide pictures of internal organs and have a fewer complications but cannot be used to treat a problem, which an ERCP is often able to do. If you have a problem in your bile duct, an operation may be an alternative to an ERCP.
What will happen if I decide not to have an ERCP?
Your doctor may not be able to confirm or treat your problem. If you are concerned about having this procedure, you should discuss this with your doctor.
The Preparation
To allow a clear view into your stomach and small intestine (Duodenum) they must be empty, so it is important not to eat for 6 hours before your appointment. You can continue with sips of water up to 2 hours before your appointment time.
During the Procedure
In the examination room you will be asked to lie on your stomach with your left arm down your side and your right arm up by your head, you will need to turn your head to face the right side. A small clip will be placed on your finger to monitor your pulse rate and oxygen levels during the procedure.
A small sponge will be placed just inside your nose to give you oxygen throughout the procedure and a mouth guard will be placed in your mouth to protect your teeth.
To ensure that you are relaxed and pain free you will receive a sedative and pain relieving injection which will make you sleepy.
The endoscope will be passed through your mouth down into the stomach and the first part of your small bowel (the duodenum) at the point where the bile duct and pancreatic duct drain into the small bowel. A dye which will show up on the x-rays, is injected via a small tube which will be passed through the endoscope, into the bile duct. Pictures can then be taken.
There are then a range of therapies that can be undertaken such as removal of Gall Stones and Stenting. The dye passes from your body harmlessly.
When will I go back to the ward?
You will be monitored in recovery until your observation is stable. The nurse from the ward will come and collect you. You will be observe closely for complication such a Haemorrhage, Pancreatitis and Perforation. The nurse or doctor in the ward will explain the outcome of your procedure and discuss any changes of medication and further investigations or appointments you may require.
Lifestyle changes
If you smoke, stopping smoking will improve your long-term health. Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight. Regular exercise should improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
Summary
An ERCP is usually a safe and effective way of treating a problem within your bile and pancreatic duct. However, complications can happen. You need to know about them to help you make an informed decision about the procedure. Knowing about them will also help to detect and treat any problems early.
Some information, such as risk and complication statistics, is taken from global studies and/or databases. Please ask your doctor for more information about the risks that are specific to you. This document is intended for information purposes only and should not replace advice that your relevant healthcare team would give you.
