Please see letter for appointment details
Please telephone the Endoscopy department on 01234 792269 if this is not convenient for you.
Please contact 07392 126603 if you would like to discuss any aspects of the procedure before your appointment.
If you have not attended a Pre Assessment appointment you will receive a phone call for you to be pre assessed over the phone. This may come through as an unknown number.
Introduction
You have been advised by your GP or hospital doctor to have an investigation known as a gastroscopy (OGD). We will need to have your formal consent before we can carry out this examination. This leaflet explains how the examinations are carried out and what the risks are. This will help you to make an informed decision when agreeing to the examinations.
What is an OGD?
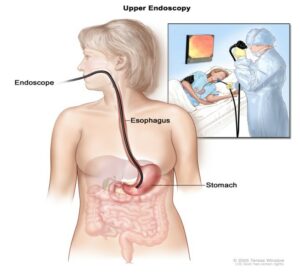
The procedure you will be having is called an oesophagogastro- duodenoscopy (OGD), simply called a gastroscopy or OGD. Gastroscopy is a procedure, which allows the doctor to examine your oesophagus (gullet), stomach and the first part of your small bowel (duodenum). A long thin flexible tube with a small video chip built into its tip, called a gastroscope is used for this procedure. Each gastroscope has an illumination channel which enables light to shine directly onto the lining of your upper digestive tract and another which relays pictures onto a television screen.
During the investigation the endoscopist may need to take some tissue samples (biopsies) from the lining of your upper digestive tract for analysis, this is painless. The samples will be looked at under a microscope in our laboratories. Photographs may be taken for your records.
Why do I need to have an OGD?
You have been advised to have this investigation to try and find the cause of your symptoms, help with treatment and if necessary, to decide on further investigation.
There are many reasons for this investigation including:
- Indigestion
- Anaemia
- Weight loss
- Vomiting
- Passing black motions (malaena)
- Vomiting blood (haematemesis)
- Difficulty swallowing
Are there any alternative procedures?
Your doctor has recommended OGD as it is the best way of diagnosing most problems with you upper digestive system.
A barium meal is an x-ray test of your upper digestive system. This test is not as accurate as an OGD, and if your doctor finds problem, you may still need an OGD to perform biopsies or provide the treatment. A Urea breath test can be used to detect a germ (helicobacter pylori) that can cause stomach ulcers.
What will happen if I decide not to have an OGD?
Your doctor may not be able to confirm what the problem is. If you decide not to have this procedure, you should discuss this carefully with your doctor.
Potential Risks
A Gastroscopy (OGD) is a safe examination for most people. Serious problems are rare, but life threatening complication are possible. However, you need to weigh up the benefits against the risks of having the procedure. There can be risks from having the examination itself, as well as from the sedation. The main risks are:
- A tear (perforation) in the lining of the bowel. Nationally this happens to approximately 1 in 10 000 people. The risk is higher if there is an abnormal narrowing (Stricture) which is stretched (dilated). You would need to be admitted to the hospital for further treatment.
- Risk of a missed lesion – Although Gastroscopy has been selected as the best test to diagnose your symptoms, no test is perfect. There is a risk of 1 in 100 that we might miss a large polyp or other important finding during your test.
- Bleeding where we take a sample (biopsy) or have removed a polyp happens very rarely, but this is usually minor and often stops on its own.
- Short Term problems with breathing, heart rate and blood pressure (related to sedation) 1 in 100. We will monitor you carefully so that if any problems do occur they can be treated quickly. Older people and those with significant health problems (for example, people with serious breathing difficulties) may be at higher risk.
- Heart Attack or Stroke (related to sedation) 1 in 5000
- There is a slight risk of damage to your teeth, crowns or bridgework (this is very rare) so please tell the nurse if you have crowns, bridgework, or loose teeth. The plastic mouthpiece used during the procedure will protect your teeth.
- Infection. It is possible to get an infection from the equipment used. The equipment is disinfected so the risk is low.
- Sore throat. This gets better quickly.
- Allergic reaction to the equipment, materials or medication. Let the team know if you have any allergies, or if you have reacted to any medication or tests in the past.
Pre Assessment Appointment
Once you have a booking date you will be pre-assessed over the phone. Please ensure you have contact details of your next of kin, escort and a list of your medicines to hand. The nurse will go into detail about the procedure, check your medical history and answer any questions you may have.
Preparation
You must not have anything to eat six hours before the examination. Sips of water are safe up to 2 hours before the test. This is to make sure your stomach is empty for proper diagnosis and treatment. It will also make the procedure more comfortable.
Medication
Your routine medication can be taken with sips of water but this will be discussed at Pre-Assessment.
If you take blood-thinning tablets such as Warfarin, Clopidogrel, Edoxaban etc., please let the endoscopy unit know at least 7 days before the procedure unless instructions have been given to you by your doctor or you were already instructed during your telephone pre-assessment.
Diabetic medication:
If you are taking medication to control your diabetes (insulin or medication) please ensure the Endoscopy Unit is aware so that your appointment can be made at the beginning of the list.
You will be told what to do with regards to your medication at your pre-assessment or telephone pre-assessment.
What happens when I arrive?
When you arrive, please book in at reception. You will then be called into the admission area where a nurse/assistant practioner will ask you to confirm your details. You will also be able to ask any questions you may have. If there are any changes to your medical condition since we did the telephone pre-assessment, please inform the admitting nurse.
The nurse will ensure you understand the procedure and you will be offered the choice of throat spray or sedation.
If you have sedation, the nurse will insert a small cannula into the back of your hand or arm during the admission to make you ready before you go to the procedure room.
If you have sedation you will not be permitted to drive home or use public transport on your own, so you must arrange for someone to collect you from the hospital and stay with you for 12 hours.
The nurse will need to be given their contact details so that they can contact them when you are ready for discharge. We advise that your escort phones the department on arrival so we can take you to them.
Your blood pressure and heart rate will be recorded and if you are diabetic, your blood glucose level will also be recorded.
Throat spray or sedation?
You will be given the choice of whether you wish to have the examination performed with a local anaesthetic spray or sedation. If you wish to have the examination performed under local anaesthetic the doctor will spray the back of your throat to make it all numb, this helps to reduce the gag reflex prior to the doctor passing the endoscope down into your gullet. Once the procedure is complete you will be able to eat and drink after 30 minutes of having the throat spray. You will then be able to leave the endoscopy unit unaccompanied, as you will be awake throughout the procedure.
Sedation will involve giving you an injection into your vein that may make you drowsy and relaxed but not unconscious. You will be in a state called conscious sedation: this means that although you are drowsy you will still hear what is said to you and therefore be able to follow simple instructions during the investigation.
Once the procedure is complete the nurses will monitor you until you are fully awake. The nurse will advise you when you can eat and drink. You may need to wait to speak to the doctor.
What happens during the examination?
A gastroscopy often takes less than 10 minutes, although it may take longer if it’s being used to treat a condition.
You will be taken into the examination room, where the endoscopist and the nurses will introduce themselves and you will have the opportunity to ask any final questions.
You will be asked safety questions about you and your health prior to the procedure.
The healthcare team will monitor your heart rate, and oxygen levels using a finger clip. They will also monitor your blood pressure, when required.
You will be sitting up to spray your throat with some local anaesthetic and ask you to swallow it. This can taste unpleasant. (If you have any dentures, you will be asked to remove them first).
The nurse looking after you will then ask you to lie on your left side. You will be given a small plastic mouth guard to put between your teeth to protect them during the examination. The sedative will be injected into a vein in your arm or hand at this point and you will quickly become sleepy. If you need oxygen (usually when having sedation), the nurse will give it to you through a small tube with a sponge under your nostril. A small suction tube, rather like the one used at the dentist, will be placed in your mouth to remove any saliva or other secretions produced by your mouth during the examination. You will be able to breath normally through your nose.
The endoscopist will place a flexible telescope (gastroscope) into the back of your throat. They may ask you to swallow when the gastroscope is in your throat. This will help the scope to pass easily into your oesophagus and down into your stomach and first part of the small bowel, called the duodenum. A small amount of air will be blown into your stomach to help the endoscopist see clearly. This may be uncomfortable, but shouldn’t cause any pain.
During the procedure the doctor may take a small sample of tissue to check for any infection or inflammation. This is called a biopsy. This procedure is painless and you will probably not be aware of it being done.
If the doctor finds a narrowed area in your oesophagus, called a stricture, which may be causing difficulties in swallowing, it may be possible to provide treatment at the same time as the endoscopy. This would involve passing a small balloon down the scope to help dilate the stricture to relieve swallowing difficulties.
The endoscopic examination
When a biopsy is taken from the lining of the stomach there is a very small risk that bleeding may occur. Usually this will stop by itself. If bleeding continues you may have to stay in hospital to be observed until the bleeding stops. When a stricture is found and dilated during endoscopy there is a very slight risk that a leakage may occur at the site being treated (less than 1%). If this occurs you would have to stay in hospital. Very occasionally an operation may be required to repair any leakage.
After the procedure, how soon will I recover?
As soon as the examination has finished you will be allowed to rest for as long as necessary. Your blood pressure and heart rate will be recorded and if you are diabetic, your blood glucose will be monitored.
If you have had throat spray you will be able to leave the department once your observations have been recorded in recovery. Please note you must not eat or drink for 30 minutes after throat spray.
If you have sedation, once you have recovered from the initial effects of the sedation (approximately 30minutes), the cannula will be removed and you will be able to get dressed.
The nurse will also go through your report and the results of your procedure.
A nurse will take you to the Endoscopy discharge lounge and you will be given refreshments while you wait for your transport home. Once your escort has arrived to collect you from discharge lounge , your escort will need to sign the discharge form , being the responsible adult who will look after you in the next 12-24 hours.
How long will I be in the Endoscopy Unit?
This depends upon how quickly you recover from your examination and also how busy the unit is. You should expect to be in the unit for most of the morning or afternoon if you chose to have sedation. The unit also deals with emergencies and these will take priority over outpatient appointments. However, we will keep any delays to a minimum.
Results
Before you leave the department, a nurse or doctor will explain the findings of your examination and discuss any changes of medication and further investigations or appointments you may require, for example, if a sample (biopsy) has been taken or polyps removed for examination. The results may take 4-6 weeks and will be sent to your GP or referring consultant. Due to the effects of the sedation, many people find they forget everything that has been said to them. You may receive a written report to aid your retention of this information.
Going home
If you have had throat spray you can carry on your day as normal.
The effects of sedation can last for 24 hours so you should not undertake the following for 24 hours following your procedure:
- Drive a car
- Operate machinery
- Drink alcohol
- Sign any legally binding documents
- Be in charge of any young children
Most people feel perfectly back to normal after 24 hours.
You are advised against foreign/remote travel in the 2 week period (if you have had a polyp removed) after this procedure, please discuss any concerns with the nursing team.
It is essential that if you have had sedation, someone collects you from the hospital, and stays with you for 12 hours. If this is not possible please contact the endoscopy unit before your procedure to discuss this.
Once home it is important to rest quietly for the remainder of the day. You may resume your normal diet and prescription medication unless otherwise instructed by the doctor.
Points to Remember:
- If you are unable to keep your appointment please notify the Endoscopy unit as soon as possible
- It is our aim for you to be seen and investigated as soon as possible after your arrival. However the department is busy and your investigation may be delayed. If emergencies occur, these patients will obviously be given priority over less urgent cases.
- The hospital cannot accept any responsibility for the loss or damage of personal property during your time on these premises.
- If you have a specific requirement, need an interpreter, or any other needs; please inform us prior to your procedure date to avoid delays or cancellation. This can be discussed during your telephone pre-assessment.
Concerns
If you have any queries regarding the procedure please contact the endoscopy unit between 8am and 6pm Monday to Sunday and the nursing staff will be happy to give you information or advice.
FOLLOWING THIS PROCEDURE YOU MUST NOT DONATE BLOOD FOR 4-6 MONTHS
The reason for this is that your ability to donate blood in the future is dependent upon your diagnosis and the possibility that you might need to undergo further investigations or complete treatments. (British Society of Gastroenterology, 2019)
Summary
A gastroscopy is usually a safe and effective way of finding out if there is a problem with the upper part of your digestive system. However, complications can happen. You need to know about them to help you make an informed decision about the procedure. Knowing about them will also help to detect and treat any problems early.
Some information, such as risk and complication statistics, is taken from global studies and/or databases. Please ask your doctor for more information about the risks that are specific to you. This document is intended for information purposes only and should not replace advice that your relevant healthcare team would give you.
Additional Information
Having a procedure with a training endoscopist
Endoscopy Training at Bedford Hospital
Bedford Hospital contributes to the training of endoscopists and as a result has several trainees working in Endoscopy; this leaflet is provided to inform you about how this may affect your Endoscopy procedure, and support your decision as to whether you are happy to have a trainee perform the procedure.
Although the idea of a trainee may be unnerving it is often a very positive experience. All our Endoscopy trainees are in a structured training programme within the national guidelines. Around a quarter of Endoscopy lists at Bedford Hospital involve training of endoscopists.
Will they be supervised?
Under no circumstances are trainee Endoscopists unsupervised. Depending on the experience of the trainee, the experienced Consultant or Senior Nurse Endoscopist will be present, and supervising your Endoscopy procedure throughout or will be immediately available in the endoscopy department. If at any time you or the trainee has any difficulties the trainer can intervene. All the Endoscopy trainers at Bedford Hospital are accredited Endoscopy trainers and we regularly monitor their training skills.
Is if safe?
We carefully monitor our complication rates for Endoscopy and there is no difference in safety with a trainee Endoscopist.
Will it be more uncomfortable?
We carefully monitor patient comfort and have not found any suggestion it will be more uncomfortable.
Will it take longer?
While learning a trainee may be slower than an independent Endoscopist, however, our trainers are experienced in monitoring the length of a procedure and will take over if procedure seems prolonged. On a training list we allow a longer time for the whole Endoscopy experience, and patients often find this makes for a more relaxed atmosphere.
What should I do if I don’t want a trainee?
If you wish to let us know you are not happy to have a supervised trainee perform your procedure please inform us at least one week in advance of the procedure, so we can ensure you are not booked on a training list. The Endoscopy administrative team are on 01234 792269 or 01234 730567.
Consent forms
You will have the procedure explained to you by a nurse and the Endoscopist will come to gain your signed and informed consent. We have supplied a consent form for you to read ahead of the day.
You can read this and tick the boxes but DO NOT SIGN until after you have spoken with your Endoscopist on the day of your procedure.
