What is an OGD?
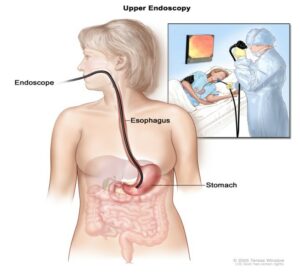
The procedure you will be having is called an oesophago-gastro-duodenoscopy (OGD), simply called a gastroscopy or OGD. Gastroscopy is a procedure, which allows the doctor to examine your oesophagus (gullet), stomach and the first part of your small bowel (duodenum). A long thin flexible tube with a small video chip built into its tip, called a gastroscope is used for this procedure. Each gastroscope has an illumination channel which enables light to shine directly onto the lining of your upper digestive tract and another which relays pictures onto a television screen.
During the investigation the endoscopist may need to take some tissue samples (biopsies) from the lining of your upper digestive tract for analysis, this is painless. The samples will be looked at under a microscope in our laboratories. Photographs may be taken for your records.
Why do I need to have an OGD?
You have been advised to have this investigation to try and find the cause of your symptoms, help with treatment and if necessary, to decide on further investigation.
There are many reasons for this investigation including:
- Indigestion
- Anaemia
- Weight loss
- Vomiting
- Passing black motions (malaena)
- Vomiting blood (haematemesis)
- Difficulty swallowing
Risks
Gastroscopy is a safe examination for most people but is classified as an invasive investigation and because of that it has the possibility of associated complications. These occur extremely infrequently; we would wish to draw your attention to them and with this information you can make your informed consent for the procedure.
The doctor who has requested this procedure will have considered this. The risk must be compared to the benefit of having the procedure carried out.
The risks can be associated with the procedure itself and with administration of sedation.
The main risks and complications are:
- Sore throat. This gets better quickly
- Allergic reaction to the equipment, materials or medication. Let the team know if you have any allergies, or if you have reacted to any medication or tests in the past.
- A tear (perforation) in the lining of the stomach, oesophagus or small bowel. This happens to approximately 1 in 3,000 people. The risk is higher if there is an abnormal narrowing (stricture) which is stretched (dilated). You will need to be admitted to the hospital for further treatment. This may be treated with antibiotics and intravenous fluids, or in very rare cases you may require surgery to repair the hole.
- Risk of missed lesion – although gastroscopy has been selected as the best test to diagnose your symptoms, no test is perfect. There is a small risk (1 in 100) that we might miss a small or large polyp or other important finding during the test. This can also happen when stomach is not clearly empty, therefore it is important to do the preparation.
- Bleeding where we take a sample (biopsy) or have removed a polyp happens to about 1 in 200 people, but this is usually minor and stops on its own.
- Sedation can occasionally cause short-term problems with breathing, heart rate and blood pressure. Careful monitoring by a fully trained endoscopy nurse ensures that the potential problems can be identified and treated rapidly. Older people and those with significant health problems may be at higher risk.
- There is a slight risk of damage to your teeth, crowns or bridgework (this is very rare) so please tell the nurse if you have crowns, bridgework, or loose teeth. The plastic mouthpiece used during the procedure will protect your teeth.
- Infection. It is possible to get an infection from the equipment used. The equipment is disinfected so the risk is low.
- Heart attack or stroke (related to sedation) can happen if you have serious medical problems – this is very rare.
Preparation
You must not have anything to eat six hours before the examination. Sips of water are safe up to 2 hours before the test. This is to make sure your stomach is empty for proper diagnosis and treatment. It will also make the procedure more comfortable.
Anticoagulant Medication:
If you are taking blood-thinning medication like Aspirin this should be stop 24 hours before the procedure.
If you are taking Warfarin or Edoxaban/ Rivoroxaban this shoud be stop 24 hours or depending on your doctor instructions. The ward staff will be able to hold this medication for you.
DIABETIC MEDICATION:
If you are taking medication to control your diabetes (insulin or medication) the ward staff will ensure that a sliding scale will be prescribe.
You will be told what to do with regards to your medication at your pre-assessment or telephone pre-assessment.
Throat spray or sedation?
You will be given the choice of whether you wish to have the examination performed with a local anaesthetic spray or sedation. If you wish to have the examination performed under local anaesthetic the doctor will spray the back of your throat to make it all numb, this helps to reduce the gag reflux prior to the doctor passing the endoscope down into your gullet. Once the procedure is complete you will be able to eat and drink after 30 minutes of having the throat spray. You will then be able to leave the endoscopy unit unaccompanied, as you will be awake throughout the procedure.
Sedation will involve giving you an injection into your vein that may make you drowsy and relaxed but not unconscious. You will be in a state called conscious sedation: this means that although you are drowsy you will still hear what is said to you and therefore be able to follow simple instructions during the investigation.
Once the procedure is complete the nurses will monitor you until you are fully awake. The nurse will advise you when you can eat and drink. You may need to wait to speak to the doctor.
What happens during the examination?
A gastroscopy often takes less than 10 minutes, although it may take longer if it’s being used to treat a condition.
You will be taken into the examination room, where the endoscopist and the nurses will introduce themselves and you will have the opportunity to ask any final questions.
You will be asked safety questions about you and your health prior to the procedure.
The healthcare team will monitor your heart rate, and oxygen levels using a finger clip. They will also monitor your blood pressure, when required.
You will be sitting up to spray your throat with some local anaesthetic and ask you to swallow it. This can taste unpleasant. (If you have any dentures, you will be asked to remove them first).
The nurse looking after you will then ask you to lie on your left side. You will be given a small plastic mouth guard to put between your teeth to protect them during the examination. The sedative will be injected into a vein in your arm or hand at this point and you will quickly become sleepy. If you need oxygen (usually when having sedation), the nurse will give it to you through a small tube with a sponge under your nostril. A small suction tube, rather like the one used at the dentist, will be placed in your mouth to remove any saliva or other secretions produced by your mouth during the examination. You will be able to breath normally through your nose.
The endoscopist will place a flexible telescope (gastroscope) into the back of your throat. They may ask you to swallow when the gastroscope is in your throat. This will help the scope to pass easily into your oesophagus and down into your stomach and first part of the small bowel, called the duodenum. A small amount of air will be blown into your stomach to help the endoscopist see clearly. This may be uncomfortable, but should not cause any pain.
During the procedure the doctor may take a small sample of tissue to check for any infection or inflammation. This is called a biopsy. This procedure is painless and you will probably not be aware of it being done.
If the doctor finds a narrowed area in your oesophagus, called a stricture, which may be causing difficulties in swallowing, it may be possible to provide treatment at the same time as the endoscopy. This would involve passing a small balloon down the scope to help dilate the stricture to relieve swallowing difficulties.
The endoscopic examination
When a biopsy is taken from the lining of the stomach there is a very small risk that bleeding may occur. Usually this will stop by itself. If bleeding continues you may have to stay in hospital to be observed until the bleeding stops. When a stricture is found and dilated during endoscopy there is a very slight risk that a leakage may occur at the site being treated (less than 1%). If this occurs you would have to stay in hospital. Very occasionally an operation may be required to repair any leakage.
After the procedure, how soon will I be sent back to the ward?
As soon as the examination has finished your blood pressure and heart rate will be recorded and if you are diabetic, your blood glucose will be monitored.
If you have had throat spray you will be able to leave the department once your observations have been recorded and stable.
If biopsies are then the results will be sent to your referring Consultant or if you were referred by your GP, they will go to the Endoscopist who completed your procedure.
If you have had sedation, once your observation is stable, then the ward will be inform to come and transfer you back. You will then be able to eat and drink once you are awake.
Results
Results and findings will be written on the report and will be sent to the ward. The ward doctor will then explain the results. If biopsies are taken, results may take 3-4 weeks and will be sent to your GP. Due to the effects of the sedation, many people find they forget everything that has been said to them. For this reason we often supply a written report.
Summary
A gastroscopy is usually a safe and effective way of finding out if there is a problem with the upper part of your digestive system. However, complications can happen. You need to know about them to help you to make an informed decision about the procedure. Knowing about them will also help to detect and treat any problems early.
Keep this information leaflet. Use it to help you if you need to talk to the healthcare team. This leaflet is intended for information purposes only and should not replace advice that your relevant healthcare team would give you.
