Please see letter for appointment details
Please telephone the Endoscopy department on 01234 792269 if this is not convenient for you.
Please contact 07392 126603 if you would like to discuss any aspects of the procedure before your appointment.
If you have not attended a Pre Assessment appointment you will receive a phone call for you to be pre assessed over the phone. This may come through as an unknown number.
Introduction
You have been advised by your GP or hospital doctor to have an investigation known as a flexible sigmoidoscopy to help find the cause of your symptoms. We will need to have your formal consent before we can carry out this examination. This leaflet explains how the examinations are carried out and what the risks are. This will help you to make an informed decision when agreeing to the examination. This leaflet may not answer all your questions so if you have any worries please don’t hesitate to ask.
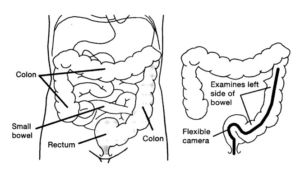
What is a Flexi-Sigmoidoscopy?
This is an examination of the left side (lower part) of the large bowel using a flexible colonoscope. The examination takes about 10-15 minutes.
You will have seen your GP or a Consultant with concerns about your bowels, for example bleeding or a change in bowel habit that does not seem to be returning back to normal. The GP or Consultant would have then referred you for this examination to find the cause of your symptoms.
If the Endoscopist thinks the bowel lining does not look normal they will use this opportunity to take tiny samples of tissue called biopsies. Sometimes small benign growths, called polyps, are found at Sigmoidoscopy. Polyps are generally removed there and then. Some polyps, if left for some years, have the potential to change into cancers.
The benefits of a Flexible Sigmoidoscopy are that it is quick and that it examines the part of the bowel where most bowel problems occur.
Why do I need to have a Flexible Sigmoidoscopy?
You have been advised to have this investigation to try and find the cause of your symptoms, help with treatment and if necessary, to decide on further investigations.
There are many reasons for this investigation including:
- Rectal Bleeding
- Altered Bowel Habit
- Abnormal Findings on previous scans
- Assessment of Inflammatory Bowel Disease (IBD)
- Polyp Surveillance
- Banding of Haemorrhoids
Alternatives to sigmoidoscopy
There are x-ray examinations which can be done instead, these can tell us if the bowel looks normal or not, but they cannot tell us what the problem is. We need to be able to take biopsies and this is not possible with x-ray. If you would like to discuss this further please speak to a member of staff.
Before your examination
Pre Assessment Appointment
Once you have a booking date you will be pre-assessed over the phone. Please ensure you have contact details of your next of kin, escort and a list of your medicines to hand. The nurse will go into detail about the procedure, check your medical history and answer any questions you may have.
Medication
Seven days before the procedure: stop taking any iron preparations. Please stop taking Aspirin when you start taking your bowel preparation.
Your procedure
Specialist doctors or nurses perform the majority of these procedures, however Bedford Hospital has commitments to train both doctors and nurses in all aspects of endoscopy and care and your test may involve Doctors or nurses training in the performance of sigmoidoscopy. Their training is provided through specialist courses and supervised by experienced consultants. If you have any queries about this please do speak to a member of the team.
The preparation
To allow a clear view, the colon must be completely empty of waste material. If it is not, certain areas may be obscured and the test may have to be cancelled or repeated. It is important to follow the detailed instructions of the laxatives about clearing the colon. Please try to follow the diet sheet provided for 3 days before you commence your bowel preparation.
It is important to take the entire laxative prescribed and also considerably increase your intake of clear fluids on the day before examination, which will help clean the bowel. You will need to be close to a toilet facility during this period, you may find a barrier cream useful, such as Sudocream or Vaseline if you become tender or sore.
If you have any issues with the bowel preparation, please contact the Endoscopy unit.
Occasionally an enema may need to be given in the department before the procedure. Sometimes your referring Doctor may decide that an enema alone is enough in which case you don’t need to take any bowel preparation. Take all your tablets as normal.
Please follow a low residue diet for 3 days before taking your bowel preparation.
What is a low fibre (residue) diet?
Dietary fibre (also known as roughage) is the part of plants that cannot be easily digested. Some of it passes through the body without being absorbed.
A low fibre (low residue) diet will help you to reduce the volume and frequency of your stools. It also lengthens the time food passes through your gut.
Eating a variety of different foods will help you get the nourishment you need to stay healthy. This leaflet gives ideas on what food to eat and also which foods to avoid while you are on a low residue diet.
WHAT FRUIT AND VEGETABLES CAN I EAT?
FRUIT
Foods allowed (limit to 1 portion per day):
- Fruit juice (no bits)
- Bananas
- Mango, papaya
- Pineapple (without the core)
- Melon, watermelon
- Fruit with the skins removed e.g. peeled apples, pears, peaches, plums, nectarines, apricots
- Pureed, stewed or cooked fruit (without skins, pips or stones)
- Tinned fruit
- Fruit sauces and coulis with pips removed e.g. sieved raspberry coulis, apple sauce
Foods to avoid:
- Fruit juice with bits
- Smoothies
- Fruits with skins on e.g. grapes, cherries, blueberries
- Citrus fruit
- Coconut
- Pineapple core
- Rhubarb
- Berries and fruits with seeds e.g. strawberries, raspberries, blackberries, kiwi,
- All dried fruit e.g. raisins
VEGETABLES
Foods allowed (limit to 1 portion per day):
- Well-cooked root vegetables e.g. carrots, parsnips, swede, turnips
- Butternut or gem squash
- Pumpkin
- Peeled marrow, courgette, squash
- Well-cooked cabbage, broccoli and cauliflower (no tough stalks)
- Peeled and de-seeded tomato, cucumber, peppers
- Avocado
- Smooth vegetable soups
- Well cooked, softened onions and garlic (as a paste)
Foods to avoid:
- All skins, pips and seeds
- Tough stalks of vegetables e.g. cauliflower, broccoli
- Raw vegetables
- Asparagus
- Aubergine
- Brussel sprouts
- Leeks, spring onions
- Raw or undercooked onions and garlic
- Pickled onions, gherkins
- Sweetcorn
- Peas, sugar snaps, mangetout
- Green, French and runner beans, broad beans
- Mushrooms
- Spring greens
- Beetroot
- Celery
- Radish
- Lettuce, rocket, watercress and spinach
- Whole tomatoes
- Bean sprouts
- Pak choi
- Soup with whole vegetables e.g. minestrone
- Chicory, fennel
- Olives
WHAT STARCHY FOODS CAN I EAT?
BREADS AND CEREALS
Foods allowed:
- Rice Krispies®, Cornflakes, Coco pops®, Frosties®, Cheerios®
- White flour, cornflour, rice flour, potato flour
- White bread, rolls, baguettes
- Seedless rye bread
- White pitta bread
- White tortilla wraps
- Crumpets, plain or cheese scones, scotch pancakes
- Croissants, brioche
- Melba toast, crackers and crispbreads (without seeds and grains)
- Rice cakes
- Plain white bagels
- Plain white
Foods to avoid:
- Wholemeal, wholegrain and bran cereals e.g. All Bran®, Branflakes®, Weetabix®
- Cereals containing dried fruit, seeds or nuts e.g. Sultana Bran®, Fruit n Fibre®, Muesli, Crunchy Nut Cornflakes®
- Special K® (all types)
- Oats, porridge, Ready Brek®
- Granola
- Wholemeal flour, wholegrain or granary flour
- Chickpea flour, cornmeal
- Wholemeal, 50/50, granary, malted, seeded or multigrain bread and bread products
- Bran
- Barley, pearl barley, spelt
- Wholegrain or seeded crackers or crispbreads
- Oat cakes
- Cereal bars containing nuts,
- Seeds and fruit
POTATO, RICE AND PASTA
Foods allowed:
- Peeled white or sweet potatoes (boiled, mashed, fried or roasted)
- Plain hash browns
- White rice
- White pasta
- Yorkshire pudding
- Pastry
- Waffles
- Rice pudding
- Couscous, bulgur wheat,
- Quinoa, gnocchi, tapioca, sago
Foods to avoid:
- Skins of jacket potatoes
- Brown and wild rice
- Wholemeal pasta
- Hash browns made with onion
WHAT PROTEIN FOODS CAN I EAT?
MEAT, FISH, POULTRY, EGGS AND MEAT SUBSTITUTES
Foods allowed:
- Most types of fish, meat and meat Products i.e. fresh, frozen, tinned
- Smooth paté and liver sausage
- Eggs
- Tofu
- Quorn
- Soya mince
- Corned beef
- Ham, gammon
Foods to avoid:
- Skin and bones of fish
- Convenience items which contain whole grains and vegetables e.g. onions, peppers
- Coarse paté made with onions
- Avoid Bacon, Sausages, Black/White Pudding
PULSES, NUTS AND SEEDS
Foods allowed:
- It is best to avoid all varieties of pulses, nuts and seeds. If you are vegetarian have a very small portion since these foods are a very good source of protein.
Foods to avoid:
- All varieties of pulses e.g. lentils, chickpeas
- All varieties of beans e.g. borlotti, cannellini, kidney, soya, baked beans and broad beans
- All nuts
- All seeds e.g. sunflower, pumpkin, sesame, poppy
- Peanut butter
- Houmous
WHAT DAIRY FOODS CAN I EAT?
Foods allowed:
- All types of milk e.g. cow’s, goat’s, sheep’s, soya, rice, oat
- Cream, crème fraiche
- Buttermilk
- All types of cheese (without dried fruit and nuts)
- Butter, margarine, spread
- Smooth yoghurt
- Ice cream and sorbet
- Custard
Foods to avoid:
- Cheese containing dried fruit or nuts
- Yoghurt containing whole fruit, nuts or seeds or pips
- Ice cream and sorbet containing nuts, seeds and whole fruits
WHAT SWEET TREATS CAN I EAT?
Foods allowed:
- Cakes made with white flour (without dried fruit or nuts)
- Plain biscuits e.g. Rich tea, shortbread
- Pancakes
- Jelly (without fruit)
- Boiled sweets
- Chocolate (without dried fruit and nuts)
- Toffee
- Jelly sweets
- Marshmallows
- Smooth nougat
Foods to avoid:
- Cakes made with wholemeal or wholegrain flour
- Cakes made with dried fruit and nuts
- Wholemeal and wholegrain biscuits e.g. Digestives, Hobnobs®
- Biscuits containing dried fruit e.g. fig rolls, Garibaldi®
- Hot cross buns, tea cakes, fruit scones
- Cereal bars containing dried fruit and nuts
- Flapjacks
- Jelly made with fresh berries
- Chocolate with nuts and dried fruit
- Nougat made with nuts and dried fruit
WHAT SAVOURY TREATS CAN I EAT?
Foods allowed:
- Crisps
- Plain bread sticks
- Cheese straws
- Mini cheddars or TUC® sandwich biscuits
- Smooth dips e.g. taramasalata, smooth guacamole
Foods to avoid:
- Nuts
- Popcorn
- Bombay Mix
- Dips that contain whole tomatoes, cucumbers, onions e.g. salsa, tzatziki
WHAT CONDIMENTS CAN I EAT?
Foods allowed:
- Tomato ketchup
- Smooth mustard
- Brown sauce
- Worcester sauce
- Soya sauce
- Mayonnaise, salad cream
- Salt and pepper
- Dried herbs
- Powdered spices
- Gravy
- Seedless jam or marmalade
- Lemon curd
- Honey
- Golden syrup, maple syrup
- Marmite®, Vegemite®, Bovril®
Foods to avoid:
- Pickles and relishes
- Chutneys
- Wholegrain mustard
- Stalks and leaves of fresh herbs
- Jam with seeds
- Marmalade with peel
- Salad dressing with wholegrain
- Mustard
On the day of the procedure
You may have as much clear fluids as you like up to 2 hours before your examination. Clear fluid is water, smooth fruit juice (not containing bits), fruit squash, fizzy drinks, tea or coffee without milk.
What happens when I arrive?
When you arrive at Reception you will be asked to take a seat to wait to be called by the admissions nurse. Once in admissions, they will explain the procedure and go through your pre assessment to make sure there have been no changes in your health. You will then be asked to get changed and prepared to see the Endoscopist. The Endoscopist will go through a consent form with you and ask you to sign it. The consent may also be obtained by a trained nurse. This is to ensure you understand the procedure and its implications and risks. If you have any worries or questions don’t be afraid to ask. The staff want you to be as relaxed as possible for the procedure and will not mind answering your queries.
A small cannula will be inserted into a vein in your arm which allows access for the doctor to give you the sedative and any other medications that may be required. Some people decline to have this procedure with sedation preferring to use other methods of pain relief such as Entonox (Gas and Air). You may still require a cannula for fluids or anti spasmodic drugs.
You will be given the choice whether to have sedation prior to the test.
During the test
A flexible sigmoidoscopy usually takes 10-15 minutes, although it may take longer if it’s being used to treat a condition.
You will be taken into the examination room, where the endoscopist and the nurses will introduce themselves and you will have the opportunity to ask any final questions.
You will be asked safety questions about you and your health prior to the procedure.
In the examination room you will be made comfortable on a couch, resting on your left side, with your knees slightly bent. A nurse will stay with you throughout the test. A small device will be attached to your finger or thumb in order to record your pulse rate and monitor your general condition during the examination and they will insert a tiny sponge into a nostril to administer oxygen, if required.
The Endoscopist will examine your bottom first with a finger, this is to feel the first few centimetres of the bowel.
When the tube has been gently inserted through the anus into the large bowel, air will be passed through it to give a clearer view of the lining. This may give you some wind-like pains but they will not last long. You may get the sensation of wanting to go to the toilet, but as the bowel is empty, there is no danger of this happening. You may pass some wind but, although this is embarrassing, remember the staff do understand what is causing it. If you are finding you have discomfort you will be offered Entonox (Gas & Air) to help relieve the pain. It usually takes up to thirty minutes for the colon to be examined, but the test sometimes lasts longer. When the examination is finished, the tube is removed safely.
Sometimes the doctor takes a biopsy – a sample of the lining for examination in the laboratory. A small piece of tissue is removed painlessly through the colonoscope, using tiny forceps. It is also possible to remove polyps during the sigmoidoscopy. Polyps are abnormal projections of tissue, which the doctor will want to examine in detail.
After the test, how soon will I recover?
After the test, you will be transferred to the recovery area where you will be continually monitored until safe for discharge, if you had sedation. If you were not given a sedative, you can normally get up straight away. You may feel a little bloated with wind pains but these usually settle quite quickly. Once you have recovered from the procedure, the cannula will be removed (if applicable) and you will be able to get dressed. The nurse will also go through your report and the results of your procedure.
A nurse will take you to the Endoscopy discharge lounge and you will be given refreshments while you wait for your transport home. Once your escort has arrived to collect you from discharge lounge, if you have sedation, your escort will need to sign the discharge form, being the responsible adult who will look after you in the next 12-24 hours.
If you had the procedure without sedation you must still not drive for 45 minutes following your last inhalation of any Entonox.
The effects of the test and injection should have worn off by the next day, however the effects of the sedation can last for 24 hours, so for this time you must not:
- Drive a car;
- Operate machinery;
- Drink alcohol;
- Sign any legal documents; or
- Be responsible for small children or other dependants
Results
As soon as the examination has finished you will be told the result and what happens next. The results may take 8-12 weeks and will be sent to your GP or referring consultant. Due to the effects of the sedation, many people find they forget everything that has been said to them. You may receive a written report to aid your retention of this information.
Potential Risks
Flexible Sigmoidoscopy is a safe examination for most people. Serious problems are rare, but life threatening complications are possible. However, you need to weigh up the benefits against the risks of having the procedure. There can be risks from having the examination itself, as well as from the sedation. The main risks are:
- A tear (perforation) in the lining of the bowel. Nationally this happens to approximately 1 in 1000 people. The risk of a tear is higher with polyp removal. If we know before your procedure that you have a large or difficult to remove polyp, your Endoscopist will discuss the risks with you in more detail. An operation may be required to repair a tear if it cannot be closed during the flexible sigmoidoscopy.
- Risk of a missed lesion – Although Flexi Sigmoidoscopy has been selected as the best test to diagnose your symptoms, no test is perfect. There is a risk of 1 in 100 that we might miss a large polyp or other important finding during your test.
- Bleeding where we take a sample (biopsy) or have removed a polyp happens to about 1 in 100 people, but this is usually minor and often stops on its own.
- Short Term problems with breathing, heart rate and blood pressure (related to sedation) 1 in 100. We will monitor you carefully so that if any problems do occur they can be treated quickly. Older people and those with significant health problems (for example, people with serious breathing difficulties) may be at higher risk.
- Heart Attack or Stroke (related to sedation) 1 in 5000
- Women taking the oral contraceptive pill should be aware that taking bowel preparation might prevent the absorption of the pill. Additional contraceptive precautions should be taken until the next period begins.
Points to Remember:
- If you are unable to keep your appointment please notify the Endoscopy unit as soon as possible
- It is our aim for you to be seen and investigated as soon as possible after your arrival. However the department is busy and your investigation may be delayed. If emergencies occur, these patients will obviously be given priority over less urgent cases.
- The hospital cannot accept any responsibility for the loss or damage of personal property during your time on these premises.
Concerns
If you have any queries regarding the procedure please contact the endoscopy unit between 8am and 6pm Monday to Sunday and the nursing staff will be happy to give you information or advice.
FOLLOWING THIS PROCEDURE YOU MUST NOT DONATE BLOOD FOR 4-6 MONTHS
The reason for this is that your ability to donate blood in the future is dependent upon your diagnosis and the possibility that you might need to undergo further investigations or complete treatments. (British Society of Gastroenterology, 2019)
Lifestyle changes
If you have any queries regarding the procedure please contact the endoscopy unit between 8am and 6pm Monday to Sunday and the nursing staff will be happy to give you information or advice.
Summary
A flexible sigmoidoscopy is usually a safe and effective way of finding out if there is a problem with your large bowel. However, complications can happen. You need to know about them to help you make an informed decision about the procedure. Knowing about them will also help to detect and treat any problems early.
Some information, such as risk and complication statistics, is taken from global studies and/or databases. Please ask your doctor for more information about the risks that are specific to you. This document is intended for information purposes only and should not replace advice that your relevant healthcare team would give you.
You are advised against foreign/remote travel in the 2 week period (if you have had a polyp removed) after this procedure; please discuss any concerns with the nursing team.
Additional information
What is Entonox?
Entonox is the trade name for the mixture of 50% Oxygen and 50% Nitrous Oxide, also known as ‘gas and air’. It is a fairly strong pain killer which works very quickly. It is often used to treat pain during childbirth, trauma and wound care. An advantage of this method of pain relief is that it is fully removed by the lungs within a few minutes after you have stopped breathing it. Entonox is safe for use in pregnancy and breastfeeding mothers.
How does Entonox work?
The exact way Entonox works is not fully understood. It is believed that once it is inhaled, Entonox travels to the brain and the spinal cord where it stops the pain from being felt.
Why is Entonox used during endoscopic procedures?
Endoscopic procedures such as flexible sigmoidoscopy and colonoscopy involve the passage of a smooth, flexible tube which has a camera on the tip, into the bowel so that the lining can be inspected. In order that the Endoscopist can view the lining, it is necessary to introduce air into the bowel through the endoscope. This can be uncomfortable and even painful for short periods. Inhaling Entonox can help to make these procedures more manageable. It may be used on its own, or in addition to intravenous (injected) sedation and analgesia if required.
What are the benefits of using Entonox?
Entonox is an effective analgesic (painkiller) which also has sedative and amnesic effects. This means that in addition to relieving pain when used for short periods, it makes the user feel temporarily drowsy, and reduces the memory of the uncomfortable experience. Entonox puts you in control of your pain relief, because it is self-administered.
Entonox wears off quickly, starting to leave your system as soon as you stop inhaling it. It has very few, mild side effects and leaves the user fit to drive within half an hour after it is last used. This can make Entonox an attractive alternative to injected sedation for those who have commitments such as work or childcare to consider.
Entonox works quickly; you may begin to feel some effect after your first few breaths. It normally takes about two minutes for Entonox to begin to work. After inhaling the gas for a couple of minutes, effective levels of pain relief should be experienced to help you cope with the discomfort of your procedure. The nursing staff will support you in the safe, continued use of Entonox as you require it during your endoscopy.
How is Entonox given?
The Endoscopy nursing staff will show you how to use the Entonox effectively and monitor and support you while you are using it. Before your procedure begins, you will be given a mouthpiece which is attached to a cylinder of Entonox gas. It is important that you hold the mouthpiece firmly between your lips to form a good seal. The nurse will moisten your lips if they are dry to help you do this. You will need to breathe deeply for one to two minutes before there is enough Entonox in your body for it to work. Entonox will only flow when you breathe in, therefore the deeper you breathe, the better your pain relief will be. You do not need to breathe Entonox for your entire procedure; only at times of pain or discomfort.
What are the risks of using Entonox?
Entonox should only be used when prescribed by a healthcare professional. There are minimal risks associated with its short-term use. If it is used repeatedly or continuously for long periods (> six to eight hours) it can affect the user’s blood count, leading to anaemia or vitamin B12 deficiency, or reduce bone marrow function. These problems are very rare and not applicable in this setting.
When Entonox is used for short periods, the main concern is that the gas may become trapped in parts of the body. This is only likely to cause problems for those with specific medical conditions. The nurses will ask you for details of your medical history and carefully assess whether it is safe for you to use Entonox. You should not use Entonox if you have:
- A recent or current ear infection, or an operation on your ears
- Recent eye surgery where injections of gas have been used
- Recently been scuba diving (within 48 hours) or have decompression sickness
- A collapsed lung or pneumothorax
- Lung disease or breathing difficulties (unstable asthma, emphysema)
- A head injury (or suspected or known increased pressure on the brain)
- A known problem with air trapped in the body (e.g., in an artery)
- A severely bloated stomach
- Injuries to the face and jaw
- Paraquat poisoning (a weedkiller)
What are the side-effects of using Entonox?
Entonox can make you feel dizzy or nauseous (sickly) but these side-effects usually settle if you slow your breathing down or stop using the gas. Some people complain of parasthesia (a tingling sensation) and light-headedness while using the gas.
If you keep breathing Entonox continuously, you will eventually become drowsy and unable to hold the mouthguard to your lips.
The nursing staff supervising you will give you some oxygen while the effects wear off, and you will wake up naturally as this happens.
Use of Entonox will also be discontinued if you start to complain of earache, if you find the side-effects unpleasant or persistent, or if you are not finding it helpful, in which case alternative pain-relieving medication may be used.
Are there any restrictions after using Entonox?
You will be monitored for half an hour after you have stopped using Entonox, until the nursing staff are happy that you have recovered and are safe to be on your own and resume your normal activities, such as driving and working.
Having a procedure with a training Endoscopist
Endoscopy Training at Bedford Hospital
Bedford Hospital contributes to the training of Endoscopists and as a result has several trainees working in Endoscopy; this leaflet is provided to inform you about how this may affect your Endoscopy procedure, and support your decision as to whether you are happy to have a trainee perform the procedure.
Although the idea of a trainee may be unnerving it is often a very positive experience. All our Endoscopy trainees are in a structured training programme within the national guidelines. Around a quarter of Endoscopy lists at Bedford Hospital involve training of Endoscopists.
Will they be supervised?
Under no circumstances are trainee Endoscopists unsupervised. Depending on the experience of the trainee, the experienced Consultant or Senior Nurse Endoscopist will be present, and supervising your Endoscopy procedure throughout or will be immediately available in the endoscopy department. If at any time you or the trainee has any difficulties the trainer can intervene. All the Endoscopy trainers at Bedford Hospital are accredited Endoscopy trainers and we regularly monitor their training skills.
Is it safe?
We carefully monitor our complication rates for Endoscopy and there is no difference in safety with a trainee Endoscopist.
Will it be more uncomfortable?
We carefully monitor patient comfort and have not found any suggestion it will be more uncomfortable.
Will it take longer?
While learning a trainee may be slower than an independent Endoscopist, however, our trainers are experienced in monitoring the length of a procedure and will take over if procedure seems prolonged. On a training list we allow a longer time for the whole Endoscopy experience, and patients often find this makes for a more relaxed atmosphere.
What should I do if I don’t want a trainee?
If you wish to let us know you are not happy to have a supervised trainee perform your procedure please inform us at least one week in advance of the procedure, so we can ensure you are not booked on a training list. The Endoscopy administrative team are on 01234 792269 or 01234 730567.
