What is a colonoscopy?
Colonoscopy is a test that allows the doctor to look directly at the lining of the large bowel (the colon) through your back passage using a flexible telescope called colonoscope.
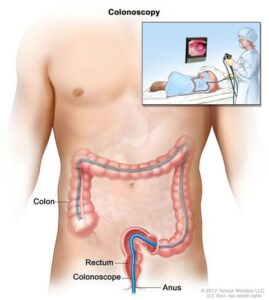
In order to carry out the test, a colonoscope is carefully passed through the rectum into the large bowel. The colonoscope is a long flexible tube, about the thickness of your index finger, with a bright light at the end. The doctor sees a clear view of the lining of the bowel and can check whether or not any disease is present. Sometimes the doctor takes a biopsy – a sample of the lining for examination in the laboratory. A small piece of tissue is removed painlessly through the colonoscope, using tiny forceps.
It is also possible to remove polyps during the colonoscopy. Polyps are abnormal projections of tissue, rather like warts, which the doctor will want to examine in detail.
Why do I need to have a Colonoscopy?
You have been advised to have this investigation to try and find the cause of your symptoms, help with treatment and if necessary, to decide on further investigation.
There are many reasons for this investigation including:
- Rectal Bleeding
- Altered Bowel Habit
- Iron Deficiency Anaemia
- Abnormal Findings
- Assessment of Inflammatory Bowel Disease (IBD)
- Polyp Surveillance
- Family History of Bowel Cancer
Are there any alternatives to a colonoscopy?
A colonoscopy is recommended as it is the best way of diagnosing most problems with your large bowel.
Other options include a CT colography (CT scan of your large bowel). However, if your doctor finds a problem, you may still need a colonoscopy to treat a problem or perform biopsies.
Medication
Ten days before the procedure: stop taking any iron preparations.
If you take Warfarin, Clopidogrel, Apixaban, or other blood – thinning medication, let the endoscopist know at least 7 days before the procedure.
Please stop taking Aspirin when you start taking your bowel preparation.
If you are diabetic and taking tablets or Insulin, The nurse will instruct when to top this or you will a sliding scale (Variable Rate insulin through a pump).
The preparation
To allow a clear view, the colon must be completely empty of waste material. If it is not, certain areas may be obscured and the test may have to be cancelled or repeated. It is important to follow the detailed instructions of the laxatives about clearing the colon. Please try to follow the diet sheet provided for 2 days before you commence your bowel preparation.
It is important to take the entire laxative prescribed and also considerably increase your intake of clear fluids on the day before examination, which will help clean the bowel. You will need to be close to a toilet facility during this period, you may find a barrier cream useful, such as Sudocream or Vaseline if you become tender or sore.
If you have any issues with the bowel preparation, please contact the Endoscopy unit.
On the day of the procedure
You may have as much clear fluids as you like up to 2 hours before your examination. Clear fluid is water, smooth fruit juice (not containing bits), fruit squash, fizzy drinks, tea or coffee without milk.
You will have to sign a Consent form. The consent may also be obtained by a trained nurse. This is to ensure you understand the procedure and its implications and risks. If you have any worries or questions don’t be afraid to ask. The staff want you to be as relaxed as possible for the procedure and will not mind answering your queries.
During the test
A colonoscopy usually takes 30-45 minutes, although it may take longer if it’s being used to treat a condition or if multiple polyps are seen.
You will be taken into the examination room, where the endoscopist and the nurses will introduce themselves and you will have the opportunity to ask any final questions.
You will be asked safety questions about you and your health prior to the procedure.
In the examination room you will be made comfortable on a couch, resting on your left side, with your knees slightly bent. A nurse will stay with you throughout the test and will monitor your heart rate, oxygen level and blood pressure. The doctor will give you a sedative injection to make you sleepy and relaxed.
The nurse will attach a small device to your finger or thumb in order to record your pulse rate and monitor your general condition during the examination and will insert a tiny sponge into a nostril to administer oxygen.
When the tube has been gently inserted through the anus into the large bowel, air will be passed through it to give a clearer view of the lining. This may give you some wind-like pains but they will not last long. You may get the sensation of wanting to go to the toilet, but as the bowel is empty, there is no danger of this happening. You may pass some wind but, although this is embarrassing, remember the staff do understand what is causing it. If you are finding you have discomfort you will be offered Entonox (Gas & Air) to help relieve the pain. It usually takes up to thirty minutes for the colon to be examined, but the test sometimes lasts longer. When the examination is finished, the tube is removed safely.
Sometimes the doctor takes a biopsy – a sample of the lining for examination in the laboratory. A small piece of tissue is removed painlessly through the colonoscope, using tiny forceps. It is also possible to remove polyps during the colonoscopy. Polyps are abnormal projections of tissue, which the doctor will want to examine in detail.
After the test, how soon will I recover?
After the test, you will be transferred to the recovery area where you will be monitored carefully.. You may feel a little bloated with wind pains but these usually settle quite quickly. We will call the ward nurse to come and take you back to ward.
You will be able to eat and drink as normal. You can also take you medication and the nurse will administer this.
