This is a break to the bone on the outside of your foot
Healing:

It can take up to 6-12 weeks for this fracture to heal.
Smoking will slow down your healing. We would advise that you stop smoking while your fracture heals. Talk to your GP or go to www.smokefree.nhs.uk for more information.
Pain and swelling:
You may have foot pain and swelling for 3-6 months after your injury. Swelling is often worse at the end of the day.
Taking pain medication, elevating your foot and using ice or cold packs will help. More information is in the next section.
Walking and your boot:
Your foot will be in a cast for 6 weeks. You are not allowed to put weight through your foot and will need to use crutches or a frame to move around.

Try to rest your foot, especially in the first 24-72 hours. Raise your foot on a stool or cushions to that it is above the level of your hip. This will help to reduce your swelling.
Exercises:
Try to maintain movement in the parts of the leg not encased in the cast by maintaining movement at the knee and hip.
Follow up:
You will receive a face to face appointment in the Fracture Clinic 6 weeks after your injury. Contact the Fracture Clinic if you have not received an appointment within 2 weeks.
DVT (deep vein thrombosis):
DVT (deep vein thrombosis) is a blood clot in a vein, usually the leg. Because you are non weight bearing, you may be at higher risk of developing a DVT. You may have been given some blood thinning medication to cover you for this period of time. However, if you are under 16, you will not be given a blood thinner unless you are taking an oral contraceptive.
Symptoms of DVT in the leg are:
- throbbing or cramping pain in 1 leg (rarely both legs), usually in the calf or thigh
- swelling in 1 leg (rarely both legs)
- warm skin around the painful area
- red or darkened skin around the painful area
- swollen veins that are hard or sore when you touch them
If you notice any of these symptoms, please call 111 immediately and get further advice or attend the Emergency Department.
Your cast:
If you have any of the following, please contact the Plaster Room (contact details can be found at the end of this leaflet).
- any new pain unrelated to your existing injury e.g. persistent burning sensation under the casts
- soreness or rubbing of the cast
- any offensive smells from the cast
- staining or leaking through the cast from a wound discharge
- the cast become broken, soft, dented or loose
- the cast becomes wet
Try to rest your ankle where possible, raise your ankle on a stool or cushions so that it is above the level of your hip. This will help to reduce your swelling.
Caring for your injury: Week 1-6
Walking and your cast
Your elbow crutches will be adjusted to the correct height, your forearms should sit within the cuff and hand grips point forward.
To stand:
- Hold the crutches in one hand by the grips
- Push up on the arm of the chair with the other hand, stand on your good leg
- Slip your arms through the arm cuffs
To sit:
- Make sure you are close to the chair so you can feel it at the back of your legs
- Get your balance on your good leg so your injured leg is off the floor
- Take your crutches off your arms
- Hold your crutches by the arm grips or lean them against the chair
- Reach back for the arms of the chair and lower yourself into the chair
- Never stand or sit with your arms in the crutches.
Walking Non Weight Bearing with elbow crutches:
- Keep your elbows into your sides
- Place the crutches forwards shoulder width apart to ensure your whole body can fit through the gap
- Lean on the crutches to take weight onto your arms and the crutches
- Step through with your good leg
- When you have your balance, repeat the above steps
Stairs – If you feel unsafe or unsteady, go up and down on your bottom.
If a handrail is available, use it and put your walking aid in the opposite hand. If you have a second crutch, hold it horizontally in the same hand.
- To go upstairs, raise your good leg up first and put your weight on it, then raise your injured leg to the same step, followed by the walking aid. Remember this when going up stairs: Good leg, injured leg, crutch, repeat.
- If going down stairs, move the crutch onto the lower step first, put your weight on the crutch as you move your injured leg onto the step alongside it. Bring your good leg onto the same step. Remember this when going down stairs: Crutch, injured leg, good leg, repeat.
Caring for your injury: Week 1-6
Exercises:
It is important to exercise your knee, hip and bottom muscles of your injured leg to maintain as much muscle strength and encourage blood flow to prevent DVTs. You should also check you can move your toes regularly. These exercises must be done without putting any weight through your injured leg. Here are some examples:
Static Quadriceps Exercise
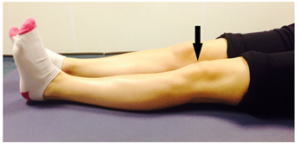
Rest with your leg supported and straight. Gently tense the muscles in your thigh and try to straighten your knee further. Hold for 5 seconds and repeat 7-10 times.
Inner Range Quads Exercise

Place a rolled up towel or small pillow under your injured knee.
Tense your thigh muscle and try to straighten your knee. Keep the back of your knee in contact with the towel/pillow.
Repeat 10 times. If you can, try to hold your knee straight for 5 seconds.
Knee Flexion and Extension
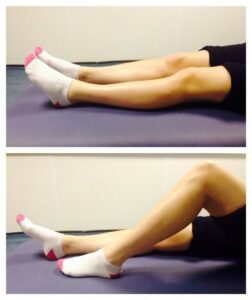
Sit or lie with your legs out stretched.
Bend and straighten your injured leg. Go as far as you feel comfortable. Repeat 7-10 times.
Seated Knee Flexion and Extension
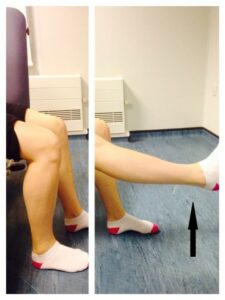
When you can do the first knee bending exercise easily, you can progress to this exercise. Sit on a chair or on the edge of your bed. Bend and straighten your knee, lifting your heel off the floor. Repeat this 10 times. If you can, try holding your knee straight for 5 seconds.
Frequently Asked Questions
I am struggling with my cast. What do I do?
If you have any pain or discomfort because of the cast please contact the plaster room.
I am diabetic, does this change things?
If you are diabetic it is very important to let us know if you have any problems with your skin. We may need to see you earlier if you are having problems. Please contact the Virtual Fracture Clinic if you have any questions.
When can I start driving?
You can return to driving when:
- You are no longer in your cast
- You can walk comfortably
- You can perform an emergency stop pain free
Always test your ability to drive in a safe environment first.
How can I get a certificate for work?
You can self-certify for the first 7 days following your injury. For any longer periods, please discuss the provision of a fitness to work statement with the Virtual Fracture Clinic Team, the Doctor at your Fracture Clinic appointment or your GP.
What do I do with my crutches or frame when I no longer need them?
Crutches can be returned to the Fracture Clinic or A&E.
I haven’t received my appointment letter. What do I do?
If you have not received your appointment letter within 2 weeks please contact the Fracture clinic.
Contact Details for Bedford and Luton
Please contact the hospital where you attended A&E as the other site will not be able to access your notes
BEDFORD HOSPITAL PATIENTS
How do I contact the Virtual Fracture Clinic (VFC)
- Telephone 01234 792036
- Messages will be checked every morning Monday to Friday (except for Bank Holidays)
- Email VFCBedford@bedfordhospital.nhs.uk
How do I contact the Fracture Clinic?
- Telephone 01234 792138
How do I contact the Plaster Room?
- Telephone 01234 792031
- Monday to Friday 9am to 5pm (out of hours contact the Emergency Department)
LUTON & DUNSTABLE HOSPITAL PATIENTS
How do I contact the Virtual Fracture Clinic (VFC)
- Telephone 01582 718121
- Messages will be checked every morning Monday to Friday (except for Bank Holidays)
- Email VFCLuton@ldh.nhs.uk
How do I contact the Fracture Clinic?
- Telephone 01582 497194 or 01582 718 993 (outpatient appointments)
How do I contact the Plaster Room?
- Telephone 01582 491166 (ext. 2233)
- Monday to Friday 9am to 5pm (out of hours contact the Emergency Department)
